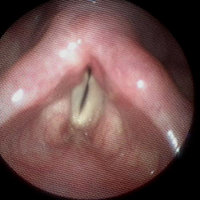
Endoscopic posterior cordotomy for treatment of dyspnea due to vocal fold immobility
Keywords:
Vocal fold immobility, posterior cordotomy, dyspnea, tracheostomyAbstract
Introduction: Several surgical procedures have been described for the treatment of respiratory distress secondary to vocal fold immobility (VFI), but the contribution of posterior cordotomy (PC) to tracheostomy weaning or prevention has not been studied in depth, particularly in the acute setting. The objective of this study was to show the effectiveness of PC to relieve dyspnea, prevent the need for tracheostomy, and enable decannulation in patients with VFI. Methods: We conducted a retrospective study and reviewed the medical records of all patients whose dyspnea warranted surgical intervention from January 2013 to January 2018. Data were retrieved on epidemiology, etiology, and duration of VFI, tracheostomy dependence, success in decannulation from tracheostomy or respiratory relief, number of procedures until decannulation, and complications. Results: Twelve suitable patients were identified of whom eleven had bilateral VFI and one had unilateral VFI. Five were tracheostomy-dependent. Ten patients underwent unilateral PC, and two patients underwent bilateral PC. All the patients experienced respiratory relief, eleven after a single PC and one after two PCs. All tracheostomy-dependent patients were decannulated. The mean follow-up after PC was 24.55 months during which none of the patients required a re-tracheostomy and three patients required revision of the PC. There were no surgical complications. Postoperatively, eight patients (67%) experienced a breathy voice and three patients (25%) had dysphagia for fluids. No patient had aspiration pneumonia. Conclusions: We conclude that PC is an easy, safe, and effective procedure for tracheostomy weaning and respiratory relief in patients with VFI. A revision PC may be indicated in some patients. A breathy voice is to be expected, and a few patients will experience dysphagia to fluids that may be addressed by instructing the patient to use a fluid thickener and take small sips.
References
Brake MK, Anderson J. Bilateral vocal fold immobility: a 13 year review of etiologies, management and the utility of the Empey index. J Otolaryngol Head Neck Surg 2015;44:1-7.
Hashmi NK, Ransom E, Nardone H, Redding N, Mirza N. Quality of life and self-image in patients undergoing tracheostomy. Laryngoscope 2010;120:S196.
Benninger MS, Gillen JB, Altman JS. Changing etiology of vocal fold immobility. Laryngoscope 1998;108:1346-50.
Pinto JA, Godoy LB, Marquis VW, Sonego TB, Leal Cde F. Bilateral vocal fold immobility: diagnosis and treatment. Braz J Otorhinolaryngol 2010;7777:594-9.
Shiki N, Olamura M, Tanabe M, Morimoto M. Differential diagnosis of hoarseness. Folia Phoniatr (Basel) 1969;21:9-23.
Hirano M. Clinical examination of voice. New York: Springer; 1981.
Segas SJ, Stavroulakis P, Manolopoulos LM, Yiotakis J, Adamopoulos G. Management of bilateral vocal fold paralysis: Experience at the University of Athens. Otolaryngol Head Neck Surg 124:1:68-71.
Dennis DP, Kashima H. Carbon dioxide laser posterior cordectomy for treatment of bilateral vocal cord paralysis. Ann Otol Rhinol Laryngol 1989;98:930-4.
Landa M, Luqui I, Gómez J, Martínez Z. Posterior cordectomy. Our experience. Acta Otorrinolaringol Esp 2013;63:26-30.
Virmani N, Dabholkar J. Laser-assisted posterior cordotomy for bilateral vocal fold paralysis: our experience. J Head Neck Physicians Surg 2016;4:23-8.
Mawaddah A, Marina MB, Halimuddin S, Mohd Razif MY, Abdullah S. A ten-year Kuala Lumpur review on laser posterior cordectomy for bilateral vocal fold immobility. Malaysian J Med Sci 2016;23:65-70.
Hillel AT, Giraldez L, Samad I, Gross J, Klein AM, Johns MM 3rd. Voice outcomes following posterior cordotomy with medial arytenoidectomy in patients with bilateral vocal fold immobility. JAMA Otolaryngol Head Neck Surg 2015;141:728–732.
Nawka T, Sittel C, Gugatschka M, Arens C, Lang-Roth R, Wittekindt C, et al. Permanent transoral surgery of bilateral vocal fold paralysis: a prospective multi-center trial. Laryngoscope 2015;125:1401-8.
Published
Issue
Section
License
Mattioli 1885 has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.




