Healthcare environments in pulmonary rehabilitation units: Effective infection control through integration of long-term antimicrobial materials
Keywords:
Contamination, antimicrobial, zinc oxide, pulmonary rehabilitation unit, infection controlAbstract
Background: Chronic obstructive pulmonary disease is a leading cause of morbidity and mortality worldwide. Effective infection control in pulmonary rehabilitation units is essential but remains insufficiently studied. This study investigated bacterial contamination, the distribution of species, and the effectiveness of antimicrobial strategies in a pulmonary rehabilitation center.
Methods: Surface swab sampling and ZnO-based antimicrobial strategies were employed to assess bacterial contamination in a pulmonary rehabilitation center. The swab samples were cultured, and species were identified.
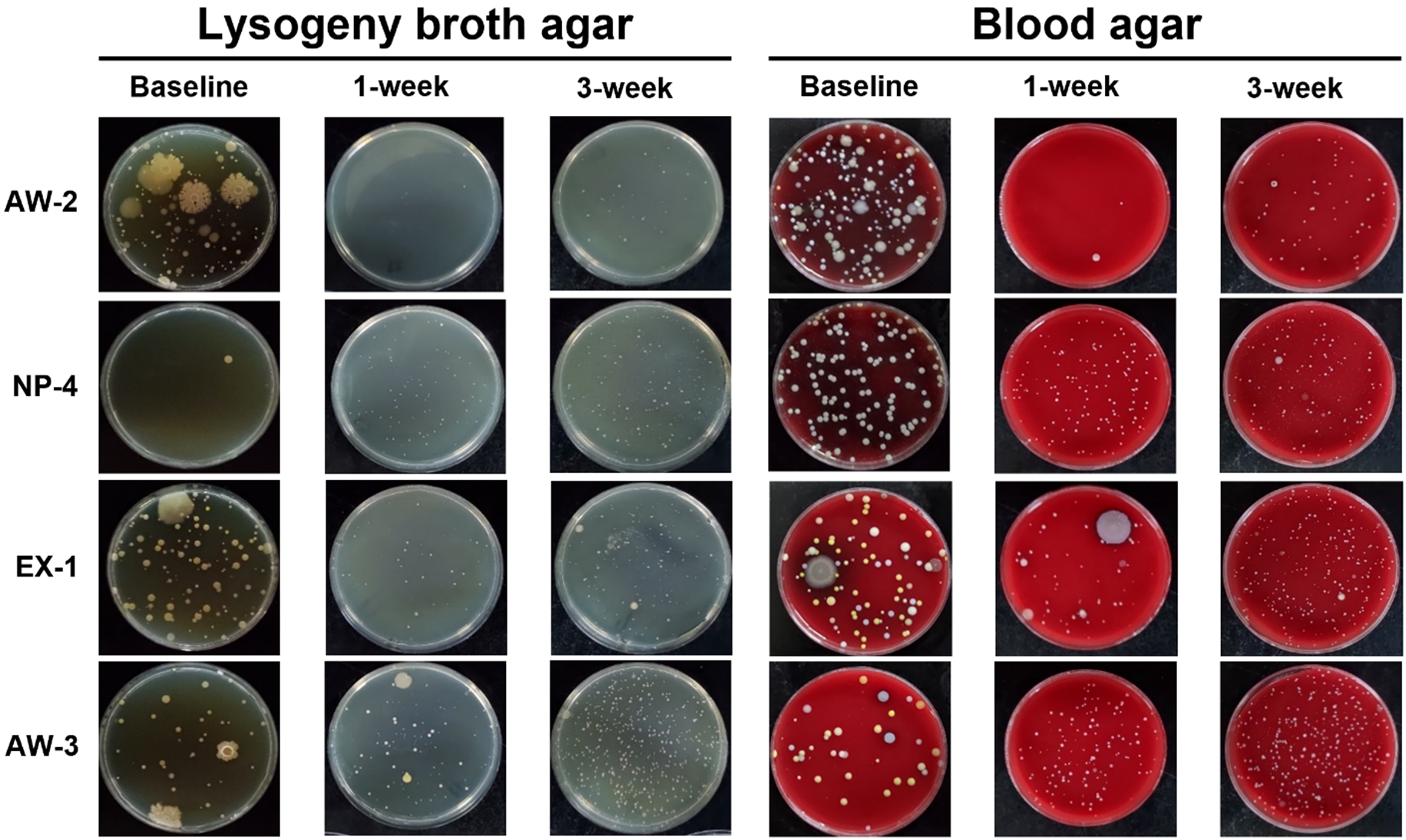
Results: Bacterial contamination on six key sampling surfaces was initially high (over 500 CFUs/100 cm2) but was significantly reduced after the application of ZnO tape to these surfaces. The antibacterial rates exceeded 80% after one week of using ZnO tape and nanoparticle suspension; however, on some surfaces, the effectiveness declined even after three weeks. These findings suggest that antibacterial protection should be renewed weekly to maintain its efficacy.
Conclusions: The application of ZnO tape and nanoparticle solution effectively reduced bacterial contamination in a pulmonary rehabilitation center, underscoring the need for regular disinfection and innovative infection control strategies.
References
1. Mathers CD, Loncar D. Projections of global mortality and burden of disease from 2002 to 2030. PLoS Med 2006; 3:e442.
2. Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 380:2095-128.
3. Vos T, Flaxman AD, Naghavi M, Lozano R, Michaud C, Ezzati M, et al. Years lived with disability (YLDs) for 1160 sequelae of 289 diseases and injuries 1990-2010: a systematic analysis for the global burden of disease study 2010. Lancet 2012; 380:2163-96.
4. Bhat TA, Panzica L, Kalathil SG, Thanavala Y. Immune dysfunction in patients with chronic obstructive pulmonary disease. Ann Am Thorac Soc 2015; 12 Suppl 2:S169-75.
5. Dong LL, Liu ZY, Chen KJ, Li ZY, Zhou JS, Shen HH, Chen ZH. The persistent inflammation in COPD: is autoimmunity the core mechanism? Eur Respir Rev 2024; 33.
6. Cosio MG, Saetta M, Agusti A. Immunologic aspects of chronic obstructive pulmonary disease. N Engl J Med 2009; 360:2445-54.
7. Kalathil SG, Lugade AA, Pradhan V, Miller A, -Parameswaran GI, Sethi S, Thanavala Y. T-regulatory cells and programmed death 1+ T cells contribute to effector -T-cell dysfunction in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2014; 190:40-50.
8. Rovina N, Koutsoukou A, Koulouris NG. Inflammation and immune response in COPD: where do we stand? -Mediators Inflamm 2013; 2013:413735.
9. Sapey E, Stockley RA. COPD exacerbations. 2: aetiology. Thorax 2006; 61:250-8.
10. Handwashing Liaison Group. Hand washing. BMJ 1999; 318:686.
11. Hilburn J, Hammond BS, Fendler EJ, Groziak PA. Use of alcohol hand sanitizer as an infection control strategy in an acute care facility. Am J Infect Control 2003; 31:109-16.
12. Nguyen DB, Gutowski J, Ghiselli M, Cheng T, Bel -Hamdounia S, Suryaprasad A, et al. A large outbreak of hepatitis C virus infections in a hemodialysis clinic. Infect Control Hosp Epidemiol 2016; 37:125-33.
13. Sui YS, Wan GH, Chen YW, Ku HL, Li LP, Liu CH, Mau HS. Effectiveness of bacterial disinfectants on surfaces of mechanical ventilator systems. Respir Care 2012;57(2):250-6..
14. van Seventer JM, Hochberg NS. Principles of infectious diseases: transmission, diagnosis, prevention, and control. In: International encyclopedia of public health. edn.; 2017:22-39.
15. Griffith CJ, Malik R, Cooper RA, Looker N, Michaels B. Environmental surface cleanliness and the potential for contamination during handwashing. Am J Infect Control 2003; 31:93-6.
16. Snyder GM, Thom KA, Furuno JP, Perencevich EN, -Roghmann MC, Strauss SM, et al. Detection of -methicillin-resistant Staphylococcus aureus and -vancomycin-resistant enterococci on the gowns and gloves of healthcare workers. Infect Control Hosp Epidemiol 2008; 29:583-9.
17. Boyce JM. Hand hygiene, an update. Infect Dis Clin North Am 2021; 35:553-73.
18. Kingston L, O’Connell NH, Dunne CP. Hand hygiene--related clinical trials reported since 2010: a systematic -review. J Hosp Infect 2016; 92:309-20.
19. Kim PW, Roghmann MC, Perencevich EN, Harris AD. Rates of hand disinfection associated with glove use, patient isolation, and changes between exposure to various body sites. Am J Infect Control 2003; 31:97-103.
20. Arenas MD, Sánchez-Payá J, Barril G, García-Valdecasas J, Gorriz JL, Soriano A, et al. A multicentric survey of the practice of hand hygiene in haemodialysis units: factors affecting compliance. Nephrol Dial Transplant 2005; 20:1164-71.
21. Duong MC, McLaws ML. Dangerous practices in a hemodialysis unit in Vietnam identify from mixed methods. BMC Infect Dis 2017; 17:181.
22. Karkar A, Bouhaha BM, Dammang ML. Infection control in hemodialysis units: a quick access to essential elements. Saudi J Kidney Dis Transpl 2014; 25.
23. Akhavan O, Ghaderi E. Enhancement of antibacterial properties of Ag nanorods by electric field. Sci Technol Adv Mater 2009; 10:015003.
24. Harding F. Breast cancer: cause, prevention, cure. Tekline publishing; 2006.
25. Arshad R, Sohail MF, Sarwar HS, Saeed H, Ali I, Akhtar S, et al. ZnO-NPs embedded biodegradable thiolated bandage for postoperative surgical site infection: in vitro and in vivo evaluation. PLoS One 2019; 14:e0217079.
26. Hemmami H, Chandran D, Ben Amor I, Zeghoud S, -Mohankumar P, Bin Emran T. ZnO nanotherapeutics for the treatment of burn wounds: recent advances: correspondence. Ann Med Surg (Lond) 2023; 85:2261-3.
27. El-Saadony MT, Fang G, Yan S, Alkafaas SS, El Nasharty MA, Khedr SA, et al. Green synthesis of zinc oxide nanoparticles: preparation, characterization, and biomedical applications - a review. Int J Nanomedicine 2024; 19:12889-937.
28. Ilves M, Palomäki J, Vippola M, Lehto M, Savolainen K, Savinko T, et al. Topically applied ZnO nanoparticles suppress allergen induced skin inflammation but induce vigorous IgE production in the atopic dermatitis mouse model. Part Fibre Toxicol 2014; 11:38.
29. Wang S, Ilves M, Mäenpää K, Zhao L, El-Nezami H, Karisola P, et al. ZnO nanoparticles as potent inducers of dermal immunosuppression in contact hypersensitivity in mice. ACS Nano 2024; 18:29479-91.
30. Mendes CR, Dilarri G, Forsan CF, Sapata VdMR, Lopes PRM, de Moraes PB, et al. Antibacterial action and target mechanisms of zinc oxide nanoparticles against bacterial pathogens. Sci Rep 2022; 12:2658.
31. Wang Y, Liu J, Wang T, Liu LZ, Tian C, Cui Y, et al. Antibacterial properties and mechanism of nanometer zinc oxide composites. Food Packag Shelf Life 2023; 40:101167.
32. Jadoun S, Yáñez J, Aepuru R, Sathish M, Jangid NK, -Chinnam S. Recent advancements in sustainable synthesis of zinc oxide nanoparticles using various plant extracts for environmental remediation. Environ Sci Pollut Res Int 2024; 31:19123-47.
33. Vijayan A, Boyce JM. 100% use of infection control procedures in hemodialysis facilities: call to action. Clin J Am Soc Nephrol 2018; 13:671-3.
34. Kanamori H, Weber DJ, Flythe JE, Rutala WA. Waterborne outbreaks in hemodialysis patients and infection prevention. Open Forum Infect Dis 2022; 9:ofac058.
35. Karkar A. Infection control guidelines in hemodialysis -facilities. Kidney Res Clin Pract 2018; 37:1-3.
36. Centers for Disease Control and Prevention. Checklist: -dialysis station routine disinfection. 2023.
37. Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (standards for quality improvement reporting excellence): revised publication guidelines from a detailed consensus process. BMJ Qual Saf 2016; 25:986-92.
38. Parsons JP, Hallstrand TS, Mastronarde JG, Kaminsky DA, Rundell KW, Hull JH, et al. An official American Thoracic Society clinical practice guideline: exercise-induced bronchoconstriction. Am J Respir Crit Care Med 2013; 187:1016-27.
39. STC Nanotech Applied Science. STC long-lasting antibacterial zinc oxide tape. Accessed Mar 21, 2025. https://www.stcnexthealth.com/collections/shop/products/antimicrobial-tape
40. STC Nanotech Applied Science. STC Nanotech zinc oxide long-lasting antibacterial spray. Accessed Mar 21, 2025. https://www.stcnexthealth.com/products/stc-nanotech-%E5%AE%89%E9%8B%85%E9%95%B7%E6%95%88%E6%8A%97%E8%8F%8C%E5%99%B4%E5%8A%91
41. Kojima K, Booth CM, Summermatter K, Bennett A, Heisz M, Blacksell SD, et al. Risk-based reboot for global lab biosafety. Science 2018; 360:260-2.
42. World Health Organization. Laboratory biosafety manual, 4th edition. Dec 25, 2024. https://www.who.int/publications/i/item/9789240011311
43. Brigando G, Sutton C, Uebelhor O, Pitsoulakis N, Pytynia M, Dillon T, et al. The microbiome of an outpatient rehabilitation clinic and predictors of contamination: a pilot study. PLoS One 2023; 18:e0281299.
44. Neely AN, Maley MP. Dealing with contaminated computer keyboards and microbial survival. Am J Infect Control 2001; 29:131-2.
45. Nazeri M, Salmani Arani J, Ziloochi N, Delkhah H, -Hesami Arani M, Asgari E, et al. Microbial contamination of keyboards and electronic equipment of ICU (intensive care units) in Kashan University of medical sciences and health service hospitals. MethodsX 2019; 6:666-71.
46. Rutala WA, White MS, Gergen MF, Weber DJ. Bacterial contamination of keyboards: efficacy and functional impact of disinfectants. Infect Control Hosp Epidemiol 2006; 27:372-7.
47. Kumar R, Sharma UD, Kumar M. Nanomaterials under high temperature and high pressure. Mod Phys Lett B 2010; 24:2647-57.
48. Mohapatra S. Sterilization and disinfection. In: Essentials of neuroanesthesia. edn.; 2017:929-44.
49. Franco D, Calabrese G, Guglielmino SPP, Conoci S. Metal-based nanoparticles: antibacterial mechanisms and biomedical application. Microorganisms 2022; 10:1778.
50. Godoy-Gallardo M, Eckhard U, Delgado LM, de Roo Puente YJD, Hoyos-Nogués M, Gil FJ, et al. Antibacterial approaches in tissue engineering using metal ions and nanoparticles: from mechanisms to applications. Bioact Mater 2021; 6:4470-90.
51. Morante N, Folliero V, Dell’Annunziata F, Capuano N, Mancuso A, Monzillo K, et al. Characterization and photocatalytic and antibacterial properties of Ag- and TiOx-based (x = 2, 3) composite nanomaterials under UV irradiation. Materials (Basel) 2024; 17:2178.
52. Eckstein BC, Adams DA, Eckstein EC, Rao A, Sethi AK, Yadavalli GK, et al. Reduction of Clostridium difficile and vancomycin-resistant enterococcus contamination of environmental surfaces after an intervention to improve cleaning methods. BMC Infect Dis 2007; 7:61.
53. Zakai S, Mashat A, Abumohssin A, Samarkandi A, -Almaghrabi B, Barradah H, et al. Bacterial contamination of cell phones of medical students at King Abdulaziz University, Jeddah, Saudi Arabia. J Microsc Ultrastruct 2016; 4:143-6.
54. Hammon M, Kunz B, Dinzl V, Kammerer FJ, Schwab SA, Bogdan C, et al. Practicability of hygienic wrapping of touchscreen operated mobile devices in a clinical setting. PLoS One 2014; 9:e106445.
55. Cieszanowski A, Czekajska E, Giżycka B, Gruszczyńska K, Podgórska J, Oronowicz-Jaśkowiak A, et al. Management of patients with COVID-19 in radiology departments, and indications regarding imaging studies - recommendations of the Polish Medical Society of Radiology. Pol J Radiol 2020; 85:e209-14.
56. Huang Z, Zhao S, Li Z, Chen W, Zhao L, Deng L, et al. The battle against coronavirus disease 2019 (COVID-19): emergency management and infection control in a radiology department. J Am Coll Radiol 2020; 17:710-6.
57. Wu YH, Chen CJ, Wu HY, Chen I, Chang YH, Yang PH, et al. Plastic wrap combined with alcohol wiping is an effective method of preventing bacterial colonization on mobile phones. Medicine (Baltimore) 2020; 99:e22910.
58. Muhammad MH, Idris AL, Fan X, Guo Y, Yu Y, Jin X, et al. Beyond risk: bacterial biofilms and their regulating approaches. Front Microbiol 2020; 11:928.
59. Das S. Genetic regulation, biosynthesis and applications of extracellular polysaccharides of the biofilm matrix of bacteria. Carbohydr Polym 2022; 291:119536.
60. Sauer K, Stoodley P, Goeres DM, Hall-Stoodley L, -Burmølle M, Stewart PS, et al. The biofilm life cycle: expanding the conceptual model of biofilm formation. Nat Rev Microbiol 2022; 20:608-20.
61. Verma P, Maheshwari SK, Mathur A. A review on bacterial biofilm formation and disassembly. Int J Pharm Sci Res 2013; 4:2900.
62. Barie PS. Surgical site infections: epidemiology and prevention. Surg Infect (Larchmt) 2002; 3 Suppl 1:S9-21.
63. Andriyanto A, Solikhah S, Suryani D. The most popular air microorganisms in the operating room in Indonesia: a literature review. Promotor 2024; 7:349-54.
64. Chuang YC, Chen YC, Chang SC, Sun CC, Chang YY, Chen ML, et al. Secular trends of healthcare-associated infections at a teaching hospital in Taiwan, 1981–2007. J Hosp Infect 2010; 76:143-9.
65. Theuretzbacher U, Bush K, Harbarth S, Paul M, Rex JH, Tacconelli E, et al. Critical analysis of antibacterial agents in clinical development. Nat Rev Microbiol 2020; 18:286-95.
66. de Allori MC, Jure MA, Romero C, de Castillo ME. Antimicrobial resistance and production of biofilms in clinical isolates of coagulase-negative Staphylococcus strains. Biol Pharm Bull 2006; 29:1592-6.
67. Viale P, Stefani S. Vascular catheter-associated infections: a microbiological and therapeutic update. J Chemother 2006; 18:235-49.
68. Chen HM, Chi H, Chiu NC, Huang FY. Kocuria -kristinae: a true pathogen in pediatric patients. J Microbiol -Immunol Infect 2015; 48:80-4.
Published
Issue
Section
License
Copyright (c) 2025 The Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Mattioli 1885 has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.




