Efficacy and adherence of auto-CPAP therapy in patients with obstructive sleep apnea: a prospective study
Keywords:
Obstructive sleep apnea, Apnea-hypopnea index, Epworth, Pichot, Auto-CPAPAbstract
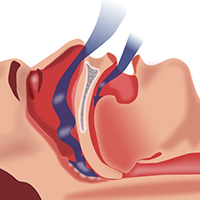
Introduction: The use of auto-continuous positive airway pressure (auto-CPAP) therapy has been recommended for subjects with moderate-to-severe obstructive sleep apnea (OSA) without significant comorbidities. This study is aimed at evaluating the efficacy and adherence of auto-CPAP therapy in subjects with OSA.
Methods: It was a perspective and descriptive study. All study subjects who had apnea-hypopnea index (AHI) >30/h, measured by polysomnography, were included. They were treated with auto-CPAP and followed-up for 6 months for evaluating the effect of CPAP-therapy on clinical and biological features and treatment adherence.
Results: One hundred and thirty-nine subjects with severe OSA were accepted for auto-CPAP therapy at inclusion. BMI was 28.4±3.8 kg/m2; neck and abdomen circumferences were 38.2±6.4 and 85.7±11.6. Epworth and Pichot scores were 18.4±6.3 and 28.3±4.5, respectively; AHI was 39±7/h and arousal index was 39±13/hour. At 6th month, 96.4% of study subjects continued to use auto-CPAP-therapy within 6.5±2.4 hours/night. There was a significant correlation between the modification (Δ) of Epworth scores and (Δ) AHI after 3 and 6 months of auto-CPAP-therapy (R=0.568 and P=0.003; R=0.745 and P=0.002; respectively). At 6th month follow-up, the main side effects of auto-CPAP were difficult sleeping, dry mouth or nose, skin marks or rashes, discomfortable breathing, and nasal congestion (36.1%, 32.0%, 20.8%, 16.0%, and 11.9%; respectively).
Conclusion: Auto-CPAP is effective in treatment of Vietnamese patients with severe OSA in short-term follow-up.
References
Peppard PE, Young T, Barnet JH, Palta M, Hagen EW, Hla KM. Increased prevalence of sleep-disordered breathing in adults. Am J Epidemiol 2013;177:1006-14.
Mirrakhimov AE, Sooronbaev T, Mirrakhimov EM. Prevalence of obstructive sleep apnea in Asian adults: a systematic review of the literature. BMC Pulm Med 2013;13:10.
Duong-Quy S, Dang Thi Mai K, Tran Van N, Nguyen Xuan Bich H, Hua-Huy T, Chalumeau F, et al. Study about the prevalence of the obstructive sleep apnoea syndrome in Vietnam. Rev Mal Respir 2018;35:14-24.
Dempsey JA, Veasey SC, Morgan BJ, O'Donnell CP. Pathophysiology of sleep apnea. Physiol Rev 2010;90:47-112.
Del Ben M, Fabiani M, Loffredo L, Polimeni L, Carnevale R, Baratta F, et al. Oxidative stress mediated arterial dysfunction in patients with obstructive sleep apnoea and the effect of continuous positive airway pressure treatment. BMC Pulm Med 2012;12:36.
Jurado-Gámez B, Fernandez-Marin MC, Gómez-Chaparro JL, Muñoz-Cabrera L, Lopez-Barea J, Perez-Jimenez F, et al. Relationship of oxidative stress and endothelial dysfunction in sleep apnoea. Eur Respir J 2011;37:873-9.
Epstein LJ, Kristo D, Strollo PJ Jr, Friedman N, Malhotra A, Patil SP, et al. Adult Obstructive Sleep Apnea Task Force of the American Academy of Sleep Medicine. Clinical guideline for the evaluation, management and long-term care of obstructive sleep apnea in adults. J Clin Sleep Med 2009;5:263-76.
Qaseem A, Holty JC, Owens DK, Dallas P, Starkey M, Shekelle P. Management of obstructive sleep apnea in adults: A clinical practice guideline from the American College of Physicians. Ann Intern Med 2013;159:471-83.
McDaid C, Durée KH, Griffin SC, Weatherly HL, Stradling JR, Davies RJ, et al. A systematic review of continuous positive airway pressure for obstructive sleep apnoea-hypopnoea syndrome. Sleep Med Rev 2009;13:427.
Sawyer AM, Gooneratne NS, Marcus CL, Ofer D, Richards KC, Weaver TE. A systematic review of CPAP adherence across age groups: clinical and empiric insights for developing CPAP adherence interventions. Sleep Med Rev 2011;15:343-56.
Weaver TE, Maislin G, Dinges DF, Bloxham T, George CF, Greenberg H, et al. Relationship between hours of CPAP use and achieving normal levels of sleepiness and daily functioning. Sleep 2007;30:711-9.
McEvoy RD, Antic NA, Heeley E, Luo Y, Ou Q, Zhang X, et al. CPAP for Prevention of Cardiovascular Events in Obstructive Sleep Apnea. N Engl J Med 2016;375:919.
Gurubhagavatula I, Sullivan S, Meoli A, Patil S, Olson R, Berneking M, et al. Management of obstructive sleep apnea in commercial motor vehicle operators: Recommendations of the AASM Sleep and Transportation Safety Awareness Task Force. J Clin Sleep Med 2017;13:745.
Morgenthaler TI, Deriy L, Heald JL, Thomas SM. The evolution of the AASM clinical practice guidelines: another step forward. J Clin Sleep Med 2016;12:129-35.
Kapur VK, Auckley DH, Chowdhuri S, Kuhlmann DC, Mehra R, Ramar K, et al. Clinical practice guideline for diagnostic testing for adult obstructive sleep apnea: an American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 2017;13:479-504.
Patil SP, Ayappa IA, Caples SM, Kimoff RJ, Patel SR, Harrod CG. Treatment of adult obstructive sleep apnea with positive airway pressure: An American Academy of Sleep Medicine clinical practice guideline. J Clin Sleep Med 2019;15:335-43.
McArdle N, Singh B, Murphy M, Gain KR, Maguire C, Mutch S, et al. Continuous positive airway pressure titration for obstructive sleep apnoea: automatic versus manual titration. Thorax 2010;65:606-11.
Hui DS, Ng SS, Tam WWS. Home-based approach is non-inferior to hospital-based approach in managing patients with suspected obstructive sleep apnoea syndrome. Am J Respir Crit Care Med.2018;197:1233-4.
Rosen CL, Auckley D, Benca R, Foldvary-Schaefer N, Iber C, Kapur V, et al. A multisite randomized trial of portable sleep studies and positive airway pressure autotitration versus laboratory-based polysomnography for the diagnosis and treatment of obstructive sleep apnea: the HomePAP study. Sleep 2012;35:757-67.
Johns MW. Sleepiness in different situations measured by the Epworth Sleepiness Scale. Sleep 1994;17:703-10.
Pichot P, Brun JP. [Questionnaire bref d'auto-évaluation des dimensions dépressive, asthénique et anxieuse].[Article in French]. Ann Mes-Psychol 1984;142:862-5.
Miller MR, Crapo R, Hankinson J, Brusasco V, Burgos F, et al. General considerations for lung function testing. Eur Respir J 2005;26:153-61.
Davies CW, Crosby JH, Mullins RL. Case-control study of 24 hour ambulatory blood pressure in patients with obstructive sleep apnoea and normal matched control subjects. Thorax 2000;55:736-40.
Parati G, Lombardi C, Hedner J. Position paper on the management of patients with obstructive sleep apnea and hypertension: joint recommendations by the European Society of Hypertension, by the European Respiratory Society and by the members of European COST (COoperation in Scientific and Technological research) ACTION B26 on obstructive sleep apnea. J Hypertens 2012;30:63346.
Pamidi S, Wroblewski K, Broussard J, Day A, Hanlon EC, Abraham V, et al. Obstructive sleep apnea in young lean men: impact on insulin sensitivity and secretion. Diabetes Care 2012;35:2384-9.
Borel AL, Monneret D, Tamisier R, Baguet JP, Faure P, Levy P, et al. The severity of nocturnal hypoxia but not abdominal adiposity is associated with insulin resistance in non-obese men with sleep apnea. PLoS One 2013;8:e71000.
Montesi SB, Edwards BA, Malhotra A, Bakker JP. The effect of continuous positive airway pressure treatment on blood pressure: a systematic review and meta-analysis of randomized controlled trials. J Clin Sleep Med 2012;8:587-96.
Fava C, Dorigoni S, Dalle Vedove F, Danese E, Montagnana M, Guidi GC, et al. Effect of CPAP on blood pressure in patients with OSA/hypopnea: a systematic review and meta-analysis. Chest 2014;145:762-71.
Schein AS, Kerkhoff AC, Coronel CC, Plentz RD, Sbruzzi G. Continuous positive airway pressure reduces blood pressure in patients with obstructive sleep apnea; a systematic review and meta-analysis with 1000 patients, J Hypertens 2014;32:1762-73.
Garcia JM, Sharafkhaneh H, Hirshkowitz M, Elkhatib R, Sharafkhaneh A. Weight and metabolic effects of CPAP in obstructive sleep apnea patients with obesity. Respir Res 2011;12:80.
Kong DL, Qin Z, Wang W, Pan Y, Kang J, Pang J. Association between obstructive sleep apnea and metabolic syndrome: a meta-analysis. Clin Invest Med 2016;39:E161-72.
Weaver TE. Don’t start celebrating – CPAP adherence remains a problem. J Clin Sleep Med 2013;9:551-2.
Weaver TE, Sawyer AM. Adherence to continuous positive airway pressure treatment for obstructive sleep apnoea: implications for future interventions. Ind J Med Res 2010;131:245-58.
Fletcher EC, Stich J, Yang KL. Unattended home diagnosis and treatment of obstructive sleep apnea without polysomnography. Arch Fam Med 2000;9:168-74.
Masa JF, Jimenez A, Duran J, Capote F, Monasterio C, Mayos M, et al. Alternative methods of titrating continuous positive airway pressure: a large multicenter study. Am J Respir Crit Care Med 2004;170:1218-24.
Published
Issue
Section
License
Mattioli 1885 has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.




