Indoor air bacterial quality and associated factors in prison inmate cells of East Hararghe Zone and Harari Regional State, Eastern Ethiopia
Keywords:
Bacterial load, Indoor air, prison inmate cell, Settle plate methodAbstract
Background: Bacterial indoor air load refers to the level of bacteria within and around dwellings and other structures. Pathogens, bacterial cell fragments, and bacterial organisms’ byproducts can all pose major issues indoors, especially in prison inmate cells. However, there is lack of data on bacterial load and contributing factors in the East Hararghe zone and Harari regional state. The lack of studies on microbiological indoor air quality in prisons with contributing factors will therefore be filled by this investigation.
Objectives: The study aimed to assess bacterial indoor air load and contributing factors in prison inmate cells from October 1 to October 30, 2020.
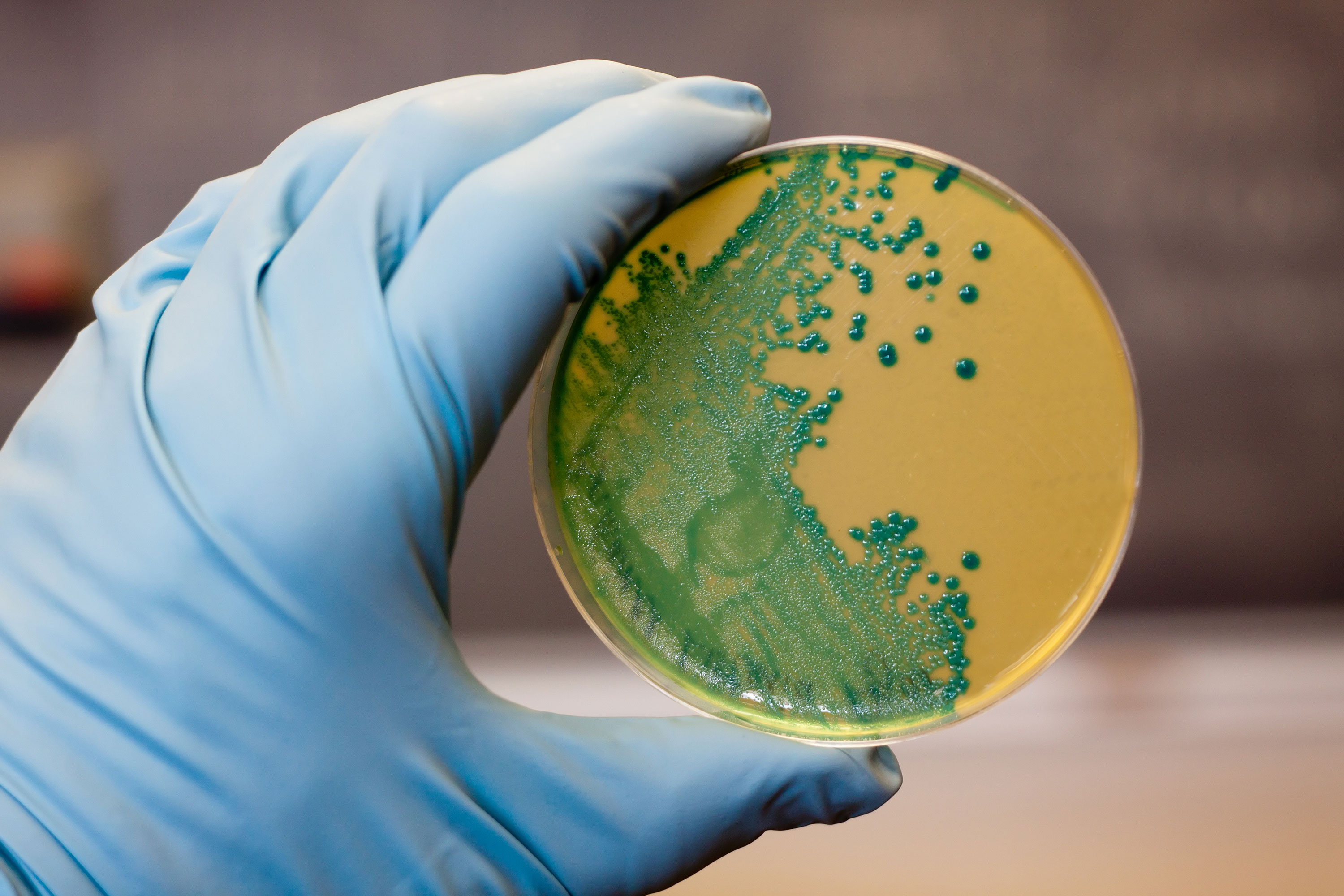
Methodology: An institutional cross-sectional study was employed. All of the prisons in the East Hararghe zone and the Harari regional state served as the study’s and source population. 62 prison cells were used in the investigation. Samples were obtained using the passively settling plate technique. The data were evaluated through the use of SPSS statistical software, Excel, and the statistical procedures of ANOVA, correlation, and chi-square test.
Results: The maximum and minimum bacterial loads, were recorded at 8:00 am (3027 CFU/m3) and 2:00 pm (1048 (CFU/m3) respectively. The correlation between the temperature and bacterial load was strongly positive (r = 0.680, p = 0.047), and the correlation of the moisture content and bacterial load was strongly negative
(r = -0.671, p = 0.039).
Conclusion: The levels of bacteria were higher than the guideline (2000 CFU/m3). While the relative humidity of indoor air was negatively correlated with bacterial load, temperature and bacterial load were significantly positively correlated. Harari regional state and East Hararghe zone prison commissions should be alarmed to alleviate these problems. The building standards need to be completely updated to the latest standards.
References
1. Haghighi MHM, Mohammadzadeh A. Microbial -Indoor Air Quality of Public Places in a Semi-dry City in Iran. Int J Trop Med 2016;11(4):102-7.
2. Bas E. Indoor air quality: A guide for facility managers. new york: The Fairmont Press, Inc.; 2004. 398 p.
3. Andualem Z, Gizaw Z, Bogale L, Dagne H. Indoor bacterial load and its correlation to physical indoor air quality parameters in public primary schools. Multidiscip Respir Med 2019;14(1):1-7.
4. World Healthorganization. The world health report 2002: reducing risks, promoting healthy life: World Health -Organization; 2002.
5. N Li N. Indoor Air Quality (IAQ): Using Temporal Data and GIS to Visualize IAQ in Campus Buildings. 2013.
6. Hänninen OO. WHO guidelines for indoor air quality: dampness and mold. InFundamentals of mold growth in indoor environments and strategies for healthy living 2011 (pp. 277-302). Wageningen Academic Publishers, -Wageningen 7 Harvey MJPJ. Living conditions of life in prisons 2018;65(1):101-2.
7. Tavoschi L, Vroling H, Madeddu G, Babudieri S, Monarca R, Vonk Noordegraaf-Schouten M, et al. Active case finding for communicable diseases in prison settings: increasing testing coverage and uptake among the prison population in the European Union/European Economic Area. Epidemiol Rev 2018;40(1):105-20.
8. Warwicker B. Desiccant materials for moisture control in buildings. InMaterials for Energy Efficiency and Thermal Comfort in Buildings 2010 Jan 1 (pp. 365-383). Woodhead Publishing
9. Otuu F, Okwuosa C, Maduka I, Ogbodo S, Shuneba I, Nkechi H, et al. Indoor Air Quality, Cell Features and Lifestyle Characteristics: Implications on the Prevalence of Some Respiratory Tract Diseases and Symptoms among Inmates of Enugu Prison, Nigeria. Advances in Clinical Toxicology 2019;4(3).
10. Ofungwu J. Indoor air quality investigation and health risk assessment at correctional institutions. Integr Environ -Assess Manag 2005;1(2):135-41.
11. Andualem Z, Gizaw Z, Dagne H. Indoor Culturable -Fungal Load and Associated Factors among Public -Primary School Classrooms in Gondar City, Northwest Ethiopia, 2018: A Cross-sectional Study. Ethiop J Health Sci 2019;29(5):623-30.
12. Andualem Z, Gizaw Z, Bogale L, Dagne H. Indoor bacterial load and its correlation to physical indoor air quality parameters in public primary schools. Multidiscip Respir Med 2019;14:2.
13. Lindsley WG, Green BJ, Blachere FM, Martin SB, Law BF, Jensen PA, Schafer MP. Sampling and characterization of bioaerosols. National Institute for Occupational Safety and Health 2017.
14. Fleischer M BGB, Bortkiewicza O, Rusiecka-Ziólkowska J. Microbiological control of airborne contamination in hospitals. Indoor and Built Environment 2006;5(1):53-6.
15. Li W, Wang S. A multi-agent based distributed approach for optimal control of multi-zone ventilation systems considering indoor air quality and energy use. Applied Energy 2020;275:115371.
16. Bonetta SA, Bonetta SI, Mosso S, Sampò S, Carraro E. Assessment of microbiological indoor air quality in an -Italian office building equipped with an HVAC system. Environ Monit Assess 2010;161(1):473-83.
17. Abdul-Wahab SA, En SC, Elkamel A, Ahmadi L, Yetilmezsoy K. A review of standards and guidelines set by international bodies for the parameters of indoor air quality. Atmospheric Pollution Research 2015;6(5):751-67.
18. Basinska M, Michalkiewicz M, Ratajczak K. Impact of physical and microbiological parameters on proper indoor air quality in nursery. Environ Int 2019;132 (61131):105098.
19. Ahmednur M, Awel H, Haile G. Microbial Indoor Air Quality and Associated Factors in Jimma Town Prison Administration, Southwestern Ethiopia. Environ Health Insights 2022;16:(1–8).
20. Landry KG, Ascension NM. Assessment of Indoor Microbial Quality of Library ‘ s Premise : Case of Central Library of the University of Yaoundé I. Open J Prev Med 2018;8:109–20.
21. Vanker A, Nduru PM, Barnett W, Dube FS, Sly PD, Gie RP, et al. Indoor air pollution and tobacco smoke exposure : impact on nasopharyngeal bacterial carriage in mothers and infants in an African birth cohort study. Respir Infect 2019;5(00052–2018). DOI: 10.1183/23120541.00052-2018
Published
Issue
Section
License
Copyright (c) 2024 The Author(s)

This work is licensed under a Creative Commons Attribution-NonCommercial 4.0 International License.
Mattioli 1885 has chosen to apply the Creative Commons Attribution NonCommercial 4.0 International License (CC BY-NC 4.0) to all manuscripts to be published.




